Intraoperative mobile cone beam CT scanner for maxillofacial surgery
Dr. Nils Petter Fossland, head of the department of maxillofacial surgery, and Dr. Mats Säll maxillofacial radiologist, at St. Olavs University Hospital, department of maxillofacial surgery, Trondheim, Norway.
The department of oral and maxillofacial surgery of St. Olavs University Hospital was established in 1962. It includes an outpatient clinic and six operating suites shared with the ear-nose-throat (ENT) department.
Expanding minimally invasive surgery for maxillofacial procedures in Norway for the past five years, Dr. Fossland, head of the department of oral and maxillofacial surgery and Dr. Säll, maxillofacial radiologist, decided to invest in a cone beam CT (CBCT) C-arm for their surgical suite. They selected OEC 3D which provides precise intraoperative CT-like volumetric images with the level of precision required for their complex maxillofacial procedures. The 3D intraoperative imaging with OEC 3D allows them to confirm a high-quality procedure before the patient’s discharge from the operating room (OR). As a result, the team decided to eliminate postoperative CT-scans.
After one year of practice with this new patient care pathway, created using intraoperative OEC 3D CT-like images, Dr. Fossland and Dr. Säll tell us what benefits they have found for their routine activity.
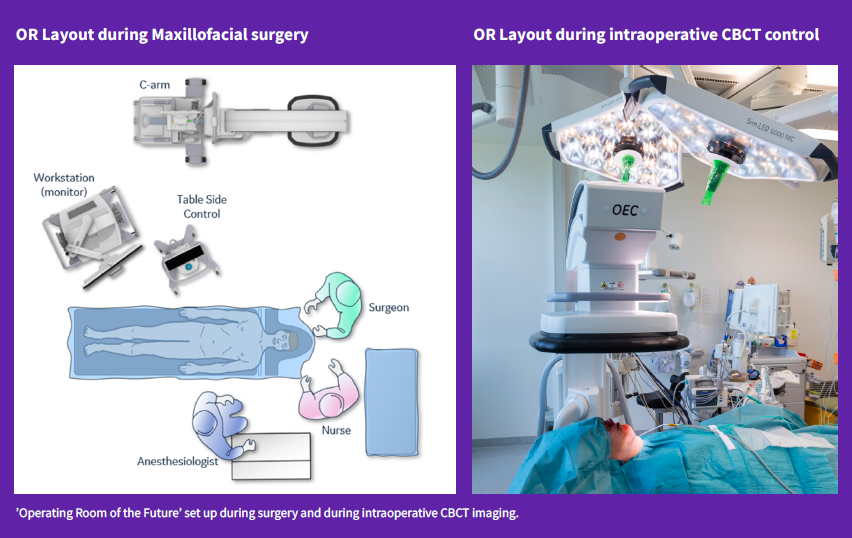
In the ‘Operating Room of the Future’ maxillofacial surgical suite, OEC 3D stands next to the patient operating table. While fluoroscopic imaging is not used in maxillofacial surgery, Dr. Fossland and Dr. Säll selected the OEC 3D C-arm to be used primarily as a mobile intraoperative CBCT imaging system. They explain why this choice allows them to avoid the postoperative CT, and how the patient benefits from a review of the surgery in the OR before discharge.
Dr. Fossland, can you explain the activities and surgical procedures of your department?
‘The oral and maxillofacial department has 6 surgeons trained and specialized in oral and maxillofacial surgery working in two dedicated ORs. Personally, I am trained both in ENT and maxillofacial surgery. However, today in Norway most maxillofacial specialists are both medical doctors and dentists who completed their training in oral and maxillofacial surgery.
Our field of expertise covers: dentoalveolar surgery (cyst and tumor treatment), dental implants, trauma surgery of the facial skeleton, orthognathic surgery (correction of bite disorders and facial asymmetries), plastic and reconstructive surgery of head, neck, and face, and open surgery of the jaw joint.
As a university hospital we have developed our expertise in these areas and have become the reference center of the region Central Norway for facial injuries, reconstructive and orthognathic surgery. We work in collaboration with orthodontists from Central Norway region, but we also receive referrals from other parts of the country for an assessment regarding surgery.
We have developed quite strong expertise in major reconstructive surgery of the head, neck, and face after traumatic injuries and cancer surgery. We have a good collaboration with both the ENT and Plastic Surgery departments here at St. Olavs University Hospital, allowing us to provide the patient with the most comprehensive care pathway possible.
Whenever possible, we want to provide a minimally invasive surgery approach. We offer endoscopic treatment of salivary gland disorders such as the removal of stones or the relief of the obstructions in the strictures of salivary gland and ducts. This is a minimally invasive operation where we enter the normal opening of the salivary gland duct with small camera and its working channel. In addition, we propose arthroscopy to diagnose and treat disorders of the temporomandibular joint (temporomandibular disorders – TMD), where this is indicated.
Over the last twelve months, our team performed about 1,100 surgical procedures. A significant part of the major surgeries is performed with OEC 3D to access intraoperative image control in the OR. Of these, there are about 75 to 100 facial fracture reduction surgeries, 50 orthodontic surgeries, 50 orbital surgeries, as well as in a smaller volume reconstructive surgery of orbital tumors and reconstructions of the temporomandibular joint (TMJ) with TMJ prosthesis.’
Dr. Fossland, can you share an example of a complex procedure where OEC 3D provides clinical benefits?
‘In orbital surgery it is very helpful to have intraoperative CT-like images because we perform very small incisions, and even while using intraoperative navigation, it can be difficult to estimate the precision of the implant placement toward the apex of the orbit.
Since we can acquire and review volumetric images during the surgery, we no longer have to wait for the postoperative examination of the patient, which is based on pain felt when moving the eye after surgery and performing a postoperative CT scan to see if the implant is one millimeter too high or not exactly where we wanted to place it with the risk of touching an eye muscle. The patient will then need to go back to surgery. Revision surgery has a cost and takes up time and resources. Now that we can access 3D images during the procedure in the OR, with a precise image quality to check the orbital implant placement, we avoid complications of revision surgery.
“I did several orbitalsurgery procedures with OEC 3D and I am very happy, OEC 3D is perfect for that.”
We estimated that about 10% of the orbital reconstruction and orthognathic procedures required revision upon review of the postoperative CBCT scan. This is how we could justify the return on investment of purchasing OEC 3D to my administration, by reducing that number of revision surgeries, over a 10-year period.
‘I believe we are quite an advanced maxillofacial department in Scandinavia. We have in our department our own preoperative CBCT scanner for diagnostics, which we acquired 6 years ago, replacing our old CBCT from 2010. We use 3D printers to create templates to plan the complex surgeries. And now we are the first maxillofacial department in Scandinavia routinely using an intraoperative mobile CBCT imaging system for a clinical application. I have heard of some colleagues in Sweden who have acquired other types of 3D C-arms, but they are not using it in their routine because it is too complicated, instead, preferring to limit its use to research in specific cases. This is why we choose OEC 3D from GE HealthCare. Our university department has a strong history of looking towards technology at the service of clinical needs.’
Dr. Säll, can you explain your role and what are the main drivers that led you to choose OEC 3D for the maxillofacial surgery OR?
‘I started my career as an intensive-care nurse as which I worked for 17 years, after which I became a dentist, working as such for 7 years, and finally I specialized in maxillofacial radiology. I have been working as a maxillofacial radiologist for 8 years now. I interpret the images and write notes for the surgeons. This is how our hospital is organized: radiologists are medically trained and specialized in different clinical domains.
Our ‘Operating Room of the Future’ project is to equip a larger operating room that we share with ENT surgeons. We are building it to satisfy the needs of different types of surgery. With this in mind, about two years ago we started to investigate the performance of 3D C-arms. We entered in communications with the different manufacturers, and we tried their C-arms.
In maxillofacial surgery, we never use C-arms for 2D fluoroscopic imaging as orthopedic surgeons do. Rather we need 3D volumetric imaging. The use of a C-arm is new to our team. I’ve trained twelve nurses in the maxillofacial OR on OEC 3D at once, and they find it very easy to use. It is significant as none of these nurses had ever been using a C-arm before! Ease of use was an important criterion. OEC 3D workflow is highly suited to the 3D acquisition and 3D image review in the OR environment. Personally, I love to review the multiplanar reconstruction (MPR) images using the oblique views. Then we send the 3D data to our PACS for further reviews. The last 3D acquisition of the procedure is used instead of the postoperative CT. This dataset is managed in our PACS along with the rest of the patient data records, as is the case for MRI or CT scan diagnostic data. The radiology department has a huge workload, so radiologists are in favor of us using this intraoperative imaging in the place of the postoperative scanner. And as I am the radiologist of the department, it is ok for the radiology department.
Of course, a main criterion in our selection was the image quality of the volumetric images since surgeons perform minimally invasive surgical techniques and work through very small incisions, using small screws and small plates. The 3D images of OEC 3D are very good.
“Indeed, in our activity, we use OEC 3D more as a mobile intraoperative scanner. ”
Sometimes we perform a 3D acquisition during the procedure, and we always perform a 3D scan at the end of the procedure to verify the position of the implants before discharging the patient. In order not to degrade the image quality of our intraoperative CT-like images obtained with OEC 3D, we are in the process of replacing all our patient tables with carbon-fiber tables over the next two years.’
Dr. Fossland, Dr. Säll what is your vision of the future for your operating room?
Dr. Säll: ‘We are working on optimizing our ‘Operating Room of the Future’ to set up the Brainlab ENT navigation system for cochlear implant placement procedures. Today this activity represents about 20 procedures per year. We expect this volume to grow once we have completed the installation. The volumetric images acquired with OEC 3D bring a good indication of the exact positioning of the tip of the electrode inside the 3 chambers of the cochlea. It is more beneficial for the patient to complete this imaging in the OR while asleep, rather than using the postoperative CBCT scanner while sitting awake, resulting in motion artifacts on the image. Thus, using OEC 3D as a mobile intraoperative scanner for the quality control of the procedure provides more information than we can get using the postoperative CBCT.
When we started the cochlear implant placement procedure with OEC 3D, I reviewed the images with another radiologist. He compared the volumetric images of the same bones of the internal ear obtained using OEC 3D with the ones obtained using the postoperative CT scanner. We concluded that OEC 3D provided images with outstanding image quality of this anatomy. As a result, there is a consensus in our team that we can start the cochlear implant placement activity with OEC 3D.
In ENT we are also interested in acquiring 3D images of the sinus to update the navigation volume intraoperatively. There are many ways to use OEC 3D in maxillofacial and ENT surgery for the benefit of the patient. We are just starting the journey!’
Dr. Fossland: ‘From the clinical point of view, we are considering broadening the use of intraoperative volumetric images for the surgical treatment of sleep apnea. In this case it makes sense to verify the alignment of the jaw before discharging the patient. OEC 3D will also be used by the ENT surgeons to confirm the intracochlear placement of cochlear implants. We have a broad range of procedures that could benefit of intraoperative volumetric CT-like images that we need to investigate.
“In our experience, the image quality of the intraoperative volumetric images of OEC 3D is better than the image quality we get with the postoperative CBCT. ”
During the postoperative CBCT acquisition, the patient stands up and the image is degraded by motion artifacts even if the acquisition duration is only 15 seconds. We have a better contrast adjustment on OEC 3D that gives a better view of the soft tissues. OEC 3D is used for final imaging, and then upon the review of the volumetric images, the surgeon can close and discharge the patient. We estimate that the patient dose with OEC 3D is one-sixth of that if the patient underwent a standard postoperative CT scan of the skull. This is a further advantage of performing intraoperative CBCT imaging with OEC 3D.
With OEC 3D, we can see some tumor contours, and in the future, it would be interesting to be able to differentiate soft tissues enough to perform measurements. For example, this would be very valuable for one of the most complex anatomies to analyze, namely the temporomandibular joint, made up of a complex structure of nerves, muscles, fibrocartilage, and a disk. A step forward in image quality would allow us to distinguish all these tissues during the operation. Today we can only access this information through a preoperative or postoperative MRI.
I really like the image resolution. I think it is better than on our postoperative CBCT that is already 5 years old. I am very impressed by how easy it is to run a 3D acquisition, the nurses do it by themselves. The nurses learned extremely fast how to perform the 3D acquisition. I just stand back and say ‘do it’. Then I review the 3D volume images on the workstation by myself.’
Reconstruction of a traumatic orbital floor with Titanium mesh implant
Courtesy of Dr. Nils Petter Fossland and Dr. Mats Säll, St Olavs University Hospital, Trondheim, Norway
Minimally invasive surgical repair of the complex anatomy and physiology of the orbital globe is an elaborated procedure that requires a precise placement of mesh to the order of a millimeter.
Patient History
The patient presented a traumatic fracture of the left orbital floor and was eligible for minimally invasive surgical reconstruction of the orbital floor by the placement of a titanium mesh implant. The procedure was performed under general anesthesia. No fluoroscopic imaging was performed during the procedure. OEC 3D was used for 3D confirmation at the end of the procedure. The intraoperative CBCT imaging allows surgeons to review the implant placement before discharging the patient, reducing the risk of potential revision surgery, and removing the need for postoperative CT imaging.
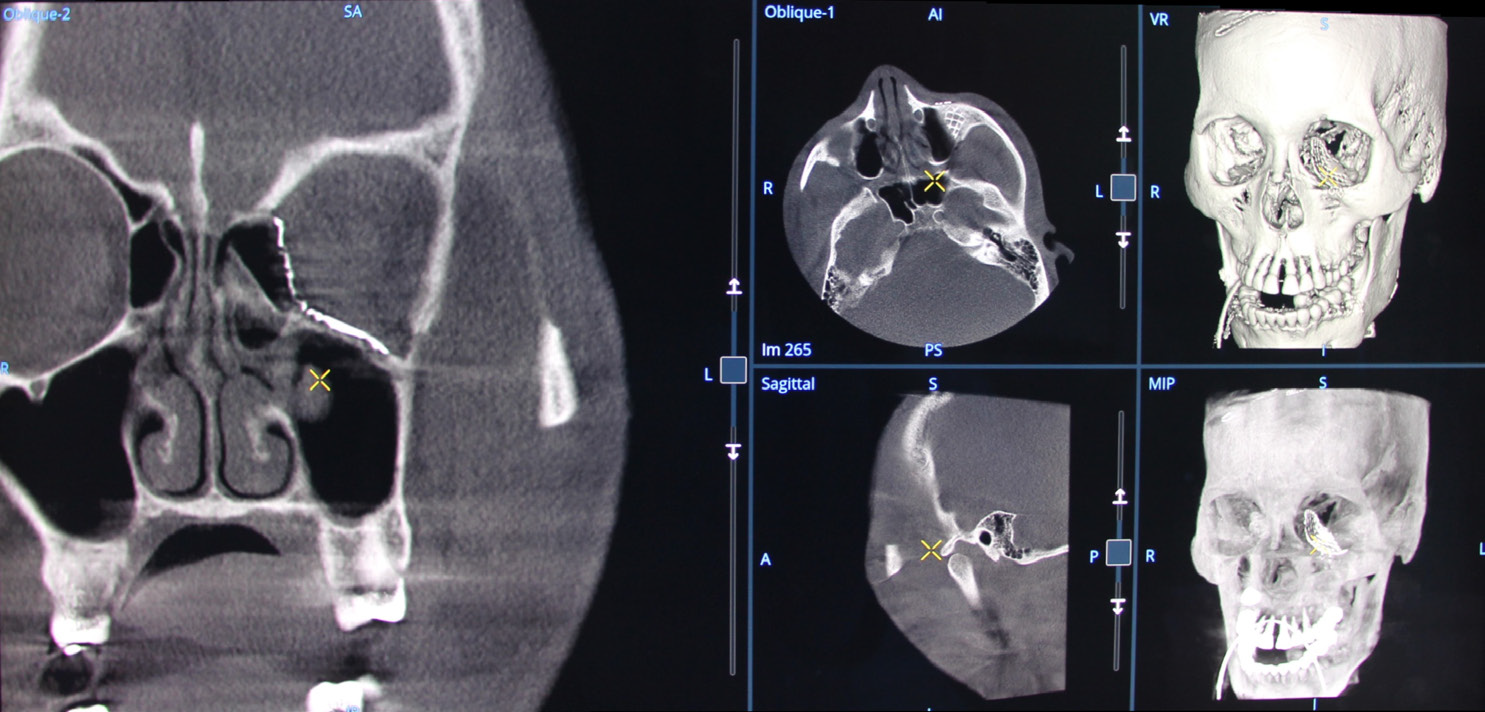
Dr. Mats Säll reviewing the final CBCT images of the procedure on the OEC 3D workstation using the 3D volume viewer.
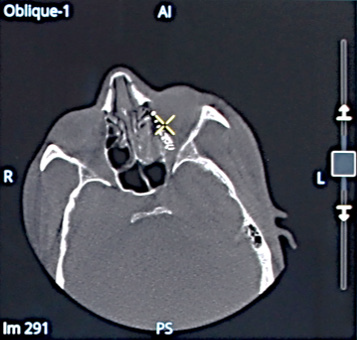
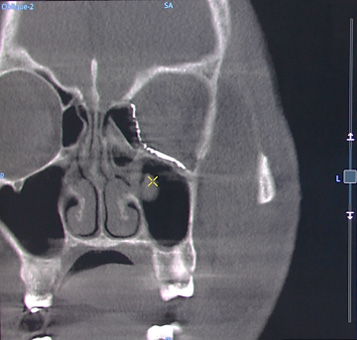
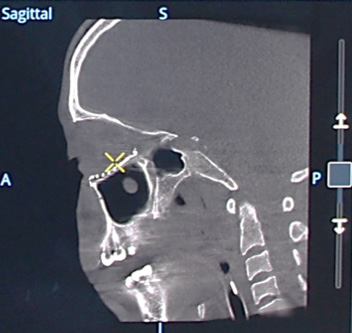
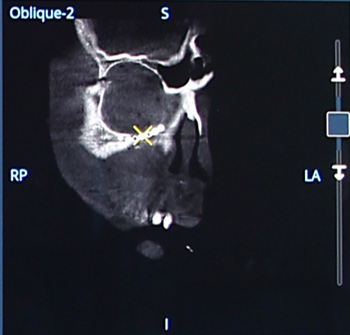
Orbital wall reconstruction with a mesh implant: volumetric images multi oblique views, Volume Rendering (VR)
and Maximum Intensity Projection (MIP).
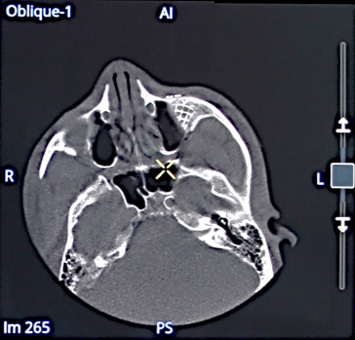
Volumetric images of the mesh in multi oblique view in axial direction.
Volumetric image of the mesh in multi oblique view in coronal and sagittal directions.
Volumetric image of the mesh in Volume Rendering format.
Right temporomandibular joint (TMJ) repair with alloplastic implant
Courtesy of Dr. Nils Petter Fossland and Dr. Mats Säll, St Olavs University Hospital,
Trondheim, Norway.
The temporomandibular joint is a complex anatomy formed by an assembly of nerves, muscles, fibrocartilage, and a disk.
Dr. Mats Säll reviewing the final CBCT images of the procedure on the OEC 3D workstation using the 3D volume viewer.
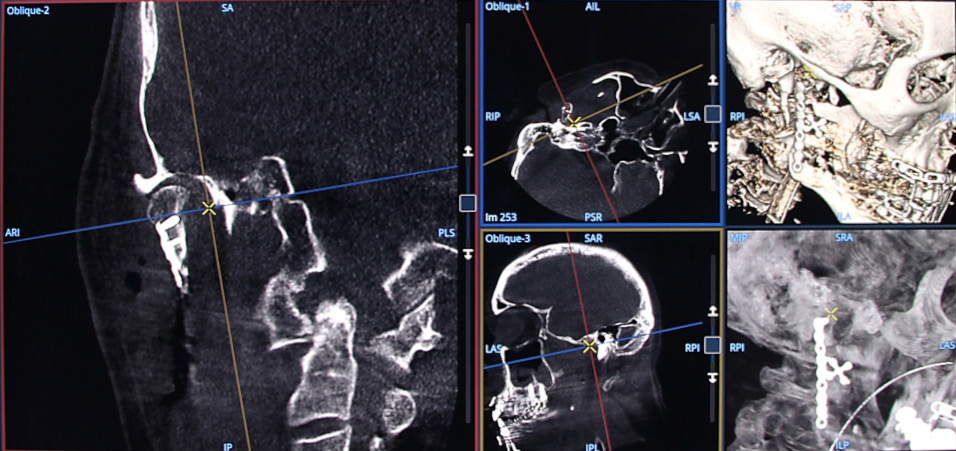
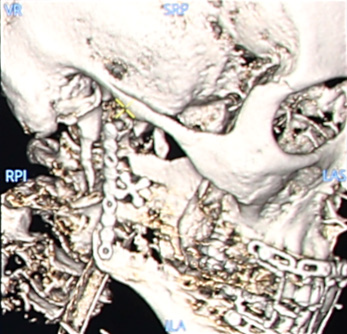
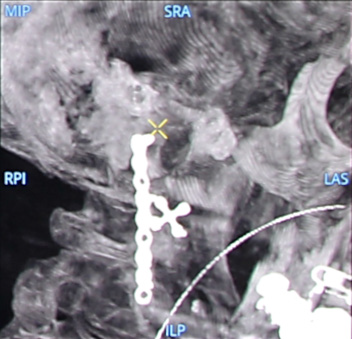
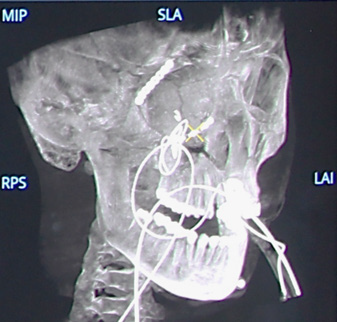
TMJ reconstruction with alloplastic implant: volumetric images in multi oblique views, Volume Rendering (VR) and
Maximum Intensity Projection (MIP).
VR (left) and MIP (right) images showing the type of implants.
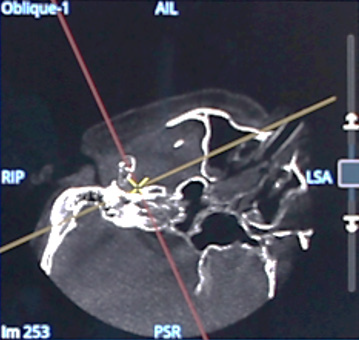
Volumetric image of the implants in the TMJ in multi oblique view in coronal and axial directions.
Right orbit fracture reduction with plate and screw fixation
Courtesy of Dr. Nils Petter Fossland and Dr. Mats Säll, St Olavs University Hospital,
Trondheim, Norway
In this case, tiny plates and screws have been placed for the reconstruction of the orbit anatomy with minimally invasive access. Final intraoperative CBCT has been performed to verify implantation.
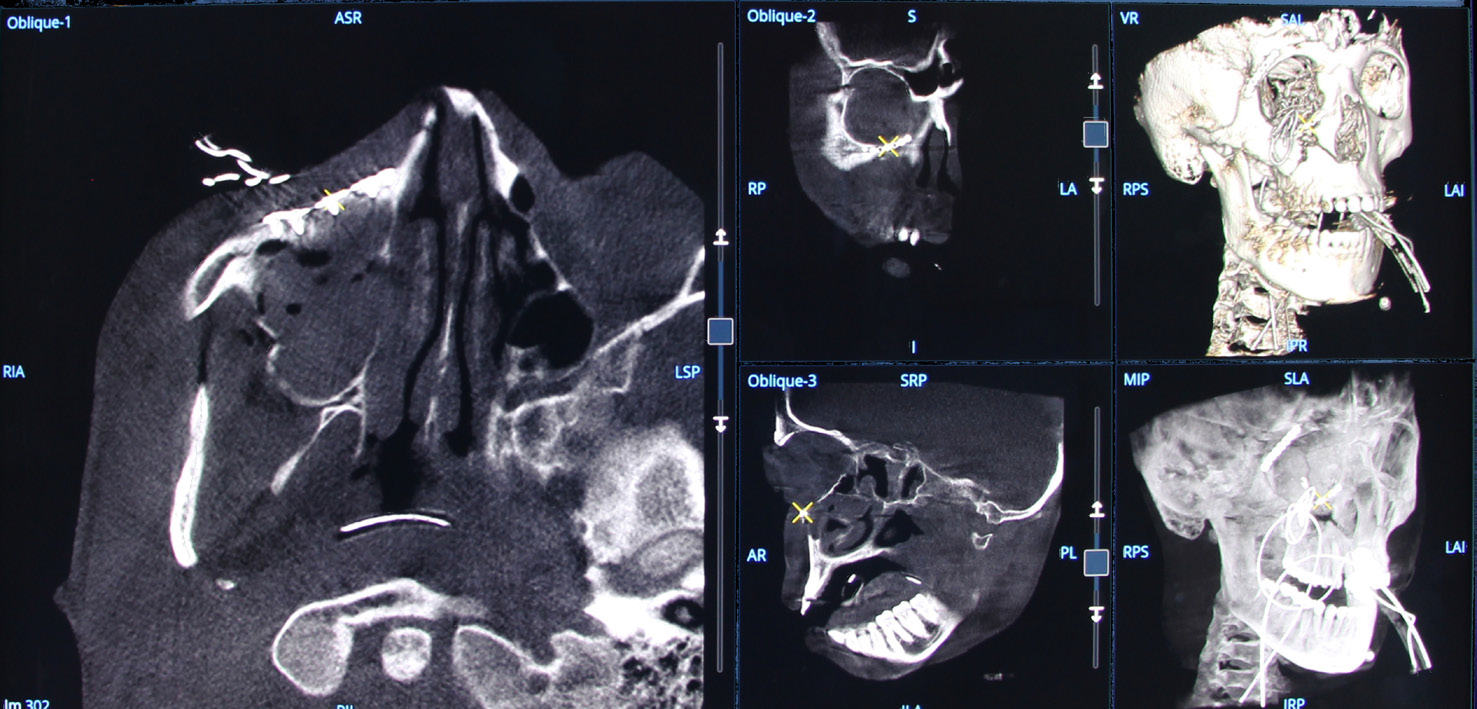
Orbit reconstruction with plates and screws: volumetric images in multi oblique views, Volume Rendering (VR) and Maximum Intensity Projection (MIP).
Volumetric image of the lower plate in multi oblique view in coronal direction.
MIP image showing the two plates in the upper and lower part of the right orbit.
REFENCES
The statements by GE HealthCare customers described here are based on their own opinions and on results that were achieved in the customer’s unique setting. Since there is no “typical” hospital and many variables exist, i.e. hospital size, case mix, etc., there can be no guarantee that other customers will achieve the same results. JB25193XX